Mammography
Mammography is a specific type of imaging that uses a low-dose x-ray system to examine breasts. A mammography exam, called a mammogram, is used to aid in the early detection and diagnosis of breast diseases in women.
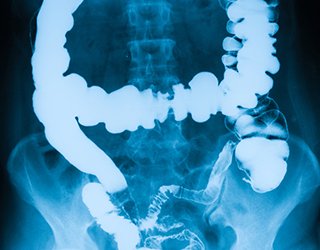
An x-ray (radiograph) is a noninvasive medical test that helps physicians diagnose and treat medical conditions. Imaging with x-rays involves exposing a part of the body to a small dose of ionizing radiation to produce pictures of the inside of the body. X-rays are the oldest and most frequently used form of medical imaging.
Three recent advances in mammography include digital mammography, computer-aided detection and breast tomosynthesis.
1. Digital mammography, also called full-field digital mammography (FFDM), is a mammography system in which the x-ray film is replaced by solid-state detectors that convert x-rays into electrical signals. These detectors are similar to those found in digital cameras. The electrical signals are used to produce images of the breast that can be seen on a computer screen or printed on special film similar to conventional mammograms. From the patient's point of view, having a digital mammogram is essentially the same as having a conventional film mammogram.
2. Digital mammography, also called full-field digital mammography (FFDM), is a mammography system in which the x-ray film is replaced by solid-state detectors that convert x-rays into electrical signals. These detectors are similar to those found in digital cameras. The electrical signals are used to produce images of the breast that can be seen on a computer screen or printed on special film similar to conventional mammograms. From the patient's point of view, having a digital mammogram is essentially the same as having a conventional film mammogram. Computer-aided detection (CAD) systems use a digitized mammographic image that can be obtained from either a conventional film mammogram or a digitally acquired mammogram. The computer software then searches for abnormal areas of density, mass, or calcification that may indicate the presence of cancer. The CAD system highlights these areas on the images, alerting the radiologist to the need for further analysis. Breast tomosynthesis, also called three-dimensional (3-D) breast imaging, is a mammography system where the x-ray tube moves in an arc over the breast during the exposure. It creates a series of thin slices through the breast that allow for improved detection of cancer and fewer patients recalled for additional imaging. systems use a digitized mammographic image that can be obtained from either a conventional film mammogram or a digitally acquired mammogram. The computer software then searches for abnormal areas of density, mass, or calcification that may indicate the presence of cancer. The CAD system highlights these areas on the images, alerting the radiologist to the need for further analysis.
3. Breast tomosynthesis, also called three-dimensional (3-D) breast imaging, is a mammography system where the x-ray tube moves in an arc over the breast during the exposure. It creates a series of thin slices through the breast that allow for improved detection of cancer and fewer patients recalled for additional imaging.
An x-ray (radiograph) is a noninvasive medical test that helps physicians diagnose and treat medical conditions. Imaging with x-rays involves exposing a part of the body to a small dose of ionizing radiation to produce pictures of the inside of the body. X-rays are the oldest and most frequently used form of medical imaging.
Three recent advances in mammography include digital mammography, computer-aided detection and breast tomosynthesis.
1. Digital mammography, also called full-field digital mammography (FFDM), is a mammography system in which the x-ray film is replaced by solid-state detectors that convert x-rays into electrical signals. These detectors are similar to those found in digital cameras. The electrical signals are used to produce images of the breast that can be seen on a computer screen or printed on special film similar to conventional mammograms. From the patient's point of view, having a digital mammogram is essentially the same as having a conventional film mammogram.
2. Digital mammography, also called full-field digital mammography (FFDM), is a mammography system in which the x-ray film is replaced by solid-state detectors that convert x-rays into electrical signals. These detectors are similar to those found in digital cameras. The electrical signals are used to produce images of the breast that can be seen on a computer screen or printed on special film similar to conventional mammograms. From the patient's point of view, having a digital mammogram is essentially the same as having a conventional film mammogram. Computer-aided detection (CAD) systems use a digitized mammographic image that can be obtained from either a conventional film mammogram or a digitally acquired mammogram. The computer software then searches for abnormal areas of density, mass, or calcification that may indicate the presence of cancer. The CAD system highlights these areas on the images, alerting the radiologist to the need for further analysis. Breast tomosynthesis, also called three-dimensional (3-D) breast imaging, is a mammography system where the x-ray tube moves in an arc over the breast during the exposure. It creates a series of thin slices through the breast that allow for improved detection of cancer and fewer patients recalled for additional imaging. systems use a digitized mammographic image that can be obtained from either a conventional film mammogram or a digitally acquired mammogram. The computer software then searches for abnormal areas of density, mass, or calcification that may indicate the presence of cancer. The CAD system highlights these areas on the images, alerting the radiologist to the need for further analysis.
3. Breast tomosynthesis, also called three-dimensional (3-D) breast imaging, is a mammography system where the x-ray tube moves in an arc over the breast during the exposure. It creates a series of thin slices through the breast that allow for improved detection of cancer and fewer patients recalled for additional imaging.
Before scheduling a mammogram, the American Cancer Society (ACS) and other specialty organizations recommend that you discuss any new findings or problems in your breasts with your doctor. In addition, inform your doctor of any prior surgeries, hormone use, and family or personal history of breast cancer.
Do not schedule your mammogram for the week before your period if your breasts are usually tender during this time. The best time for a mammogram is one week following your period. Always inform your doctor or x-ray technologist if there is any possibility that you are pregnant.
The ACS also recommends you:
Do not schedule your mammogram for the week before your period if your breasts are usually tender during this time. The best time for a mammogram is one week following your period. Always inform your doctor or x-ray technologist if there is any possibility that you are pregnant.
The ACS also recommends you:
- Do not wear deodorant, talcum powder or lotion under your arms or on your breasts on the day of the exam. These can appear on the mammogram as calcium spots.
- Describe any breast symptoms or problems to the technologist performing the exam.
- If possible, obtain prior mammograms and make them available to the radiologist at the time of the current exam.
- Ask when your results will be available; do not assume the results are normal if you do not hear from your doctor or the mammography facility.
You will feel pressure on your breast as it is squeezed by the compression paddle. Some women with sensitive breasts may experience discomfort. If this is the case, schedule the procedure when your breasts are least tender. Be sure to inform the technologist if pain occurs as compression is increased. If discomfort is significant, less compression will be used.
Benefits
- Imaging of the breast improves a physician's ability to detect small tumors. When cancers are small, the woman has more treatment options.
- The use of screening mammography increases the detection of small abnormal tissue growths confined to the milk ducts in the breast, called ductal carcinoma in situ (DCIS). These early tumors cannot harm patients if they are removed at this stage and mammography is the only proven method to reliably detect these tumors. It is also useful for detecting all types of breast cancer, including invasive ductal and invasive lobular cancer.
- No radiation remains in a patient's body after an x-ray examination.
- X-rays usually have no side effects in the typical diagnostic range for this exam.
- There is always a slight chance of cancer from excessive exposure to radiation. However, the benefit of an accurate diagnosis far outweighs the risk.
- The effective radiation dose for this procedure varies. See the Safety page for more information about radiation dose.
- False Positive Mammograms. Five percent to 15 percent of screening mammograms require more testing such as additional mammograms or ultrasound. Most of these tests turn out to be normal. If there is an abnormal finding, a follow-up or biopsy may have to be performed. Most of the biopsies confirm that no cancer was present. It is estimated that a woman who has yearly mammograms between ages 40 and 49 has about a 30 percent chance of having a false-positive mammogram at some point in that decade and about a 7 percent to 8 percent chance of having a breast biopsy within the 10-year period.
- Women should always inform their physician or x-ray technologist if there is any possibility that they are pregnant. See the Safety page for more information about pregnancy and x-rays.
Risks
A Word About Minimizing Radiation Exposure
Special care is taken during x-ray examinations to use the lowest radiation dose possible while producing the best images for evaluation. National and international radiology protection organizations continually review and update the technique standards used by radiology professionals.
Modern x-ray systems have very controlled x-ray beams and dose control methods to minimize stray (scatter) radiation. This ensures that those parts of a patient's body not being imaged receive minimal radiation exposure.
Other Guidlines